“It’s just stress.” The Unmasking of my Uterine Fibroids and Polyps
More than 80% of Black women will be diagnosed with uterine fibroids by age 50, and we are approximately twice as likely as white women to undergo more invasive surgical procedures to treat them. Bianca shares her own journey, starting with the life-threatening emergency that led to the discovery of multiple uterine fibroids and a large polyp.
Being a doctoral student (now a candidate) introduced many stressors to my life. Due to the stress of my program, what I thought was an elongated menstrual cycle turned out to be more deadly than I could ever have imagined.
4.1. That was the measure of my hemoglobin, a protein in red blood cells that carries oxygen throughout the body. For women, normal hemoglobin levels are between 12.1-15.1 grams per deciliter. Feeling extremely lightheaded and losing my breath with even the smallest step, I had my partner take me to urgent care, where I asked for a complete blood count panel (CBC). I sat in the urgent care in disbelief at what the doctor said next, “You need to go to the emergency room now. Do not delay; go.”
I remember her telling me that I set a record in her career as a physician—the lowest level of hemoglobin she had ever seen. This was something that I would hear at every doctor’s appointment moving forward. I spent almost a week in the hospital with severe and symptomatic anemia. Four bags of blood were used for my blood transfusion. I was discharged from the hospital with a level of 7.1.
Months earlier, I had visited two OB/GYNs at a top healthcare facility, the ivory tower of medical systems. I told both OB/GYNs that I was tired often and my period had not stopped for months. Every time, each OB/GYN asked me if I was stressed. Well—yes, I am in a doctoral program and working through multiple qualifying exams. “Well, it’s just the stress.” My partner and I both raised the issue of possible anemia with the second physician. They saw no signs of me needing bloodwork to rule it out. Yet I was tired, sometimes dizzy, always cold, and having shortness of breath. In the after-visit notes, the physician wrote, “appears to be in good health, alert, and sound blood pressure.” I had to ask for additional options, for which they recommended a transvaginal ultrasound. I scheduled it that day, and it was completed the following day. I never heard back from this physician about my results. Luckily, the hospital where I was admitted to treat my emergency was able to obtain my results.
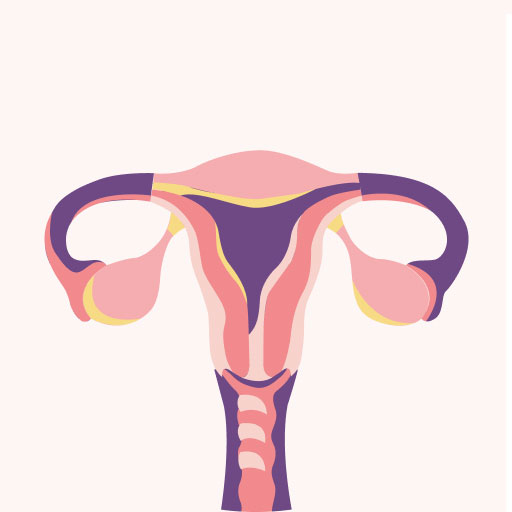
I was told I had several uterine fibroids and a large polyp that was 2.6cm in length in my uterine cavity.
There are three major types of fibroids based on location: intramural (growing within the muscular wall of the uterus), submucosal (protruding into the uterine cavity), and subserosal (pushing to the outside of the uterus). Uterine fibroids are common among Black women. More than 80% of Black women will be diagnosed with uterine fibroids by age 50. Approximately 4.2% of women are hospitalized yearly for uterine fibroids, but Black women have higher rates of hospitalization and surgical procedures. The size of uterine fibroids is often larger within Black women compared to White women. Associated with larger uterine fibroids is an increased risk for hospitalization, for which there is an increased burden of costs. Treatment options for uterine fibroids can range from noninvasive procedures (e.g., medications) to surgical procedures (e.g., myomectomy and hysterectomy). Black women are approximately twice as likely as White women to undergo open abdominal hysterectomies vs. minimally invasive hysterectomies (MIHs) to eliminate issues related to uterine fibroids. Sadly, a national hospital survey found that Black women began having hysterectomies as early as 25, compared to myomectomies with a starting age as young as 20. Research is varied as to the explanation of these racial disparities. However, this trend of Black women disproportionately having more invasive surgical treatments than their white counterparts continues to increase today.
Different Types of Hysterectomies |
|
| Total Hysterectomy | Removal of the uterus and cervix only |
| Supracervical Hysterectomy | Removal of the upper part of the uterus only, but the cervix remains |
| Total Hysterectomy with Bilateral Salpingo-Oophorectomy | Removal of the uterus, cervix, fallopian tubes (salpingectomy), and ovaries (oophorectomy). |
| Radical Hysterectomy with Bilateral Salpingo-Oophorectomy | Removal of the uterus, cervix, fallopian tubes, ovaries, the upper part of the vagina, and some surrounding tissue/ lymph nodes |
During my time in the hospital, I made necessary changes. I changed my gynecologist, primary care provider, and the overall healthcare system I went to for care. I ended up switching to the medical network of the hospital where I was treated. The hospital nurses and doctors talked to me. Actually talked to me about what had been going on—month by month, visit by visit. The recovery plan they came up with was centered around me and the options that would allow me to have children in the future. I was going to need surgery to remove the polyp. The physician wanted to take the least invasive route regarding my fibroids and warned me that if certain procedures did not work, the chance of a myomectomy AND hysterectomy increased. I was also told that by the age of 50, a hysterectomy would be needed. My doctor noted that my age, placement, and the size of the fibroids were the greatest risk factors that made these procedures my likely options.
As a 30-something-year-old, it never crossed my mind that I may ever need a hysterectomy; let alone by the age of 50. It made me think about college and how my friends and I would skip class, eat chocolate, and wear a heating pad. Boom – we made it through another cycle and went on with our lives. But in my 30s, I face the reality of surgeries, the risks associated with childbirth, and other health complications. The prospect of surgery made me think deeply about what it means to plan for children and future concerns, like a potentially weakened uterine muscle wall due to removing the fibroids.
Different Surgical Procedures for Hysterectomy |
|
| Vaginal Hysterectomy | The uterus is removed through an incision at the top of the vagina with no abdominal incisions made |
| Laparoscopic Hysterectomy / Robotic-Assisted Laparoscopic | A laparoscope is a thin device with a video camera on the end of it and is inserted in the lower abdomen through a small incision in the belly button. Several other small incisions will be made. The uterus is removed in small pieces through incisions in the abdomen or through the vagina (laparoscopic vaginal hysterectomy). For robotic-assisted laparoscopic hysterectomies, the procedure is done with the help of a robotic machine, and the robotic arms and instruments are controlled by your surgeon |
| Abdominal Hysterectomy | A 6-inch to 8-inch incision will be made, giving the surgeon a clear view of the pelvic organ. The incision is made in the abdomen, either from the belly button to the pubic bone or the top of the pubic hairline |
I was both hopeful and afraid for my uterine polypectomy. I started following the “We Can Wear White” Instagram page to understand life after polyps (and possibly uterine fibroids). I watched several of my Black college classmates post about their battle with fibroids and share information from this page. This page highlighted awareness about fibroids and lifestyle management. It was inspiring, and many stories resonated with me. I related to women who, like me, couldn’t wear anything light because of constant bleeding and fear of leaking, or who never felt secure enough to leave the house for long; in addition, there was the constant checking of the placement of the overnight pads I was wearing, and the restless nights from frequent visits to the bathroom. I also often felt isolated from the busyness of life. Post-surgery, my life feels like it’s turned around 180 degrees. Yet, I know I wouldn’t be here if I didn’t question not one but two “highly skilled and Ivy-league educated” physicians. My physician performed the polypectomy a month after my emergency hospital visit. Before I left the hospital, my pre-and-post follow-ups were already scheduled. Given my hemoglobin A1C levels, my physician did not want to delay treatment.
Advocating for your health as a Black woman can feel like going to war. And when you consider the disparity in outcomes between Black and White women dealing with the same medical issues, it can feel especially unfair. Still, this is the reality for many. Black women have similar experiences to mine every day, and though the state of our health is constantly in the news, the disparities and lack of deep concern for our health persist. Together, we can and must strive to change this, not just for ourselves but for generations of Black women to come. By sharing my story, I hope to inspire other Black women to advocate for themselves and their loved ones; our very lives depend on it.