The Complicated History of Birth Control in the African American Community: What You Really Need to Know about Birth Control
In the United States, 99 percent of women who have been sexually active report having used birth control at some point in their lives. Birth control is championed as a groundbreaking innovation that provides women with reproductive freedom to prevent pregnancy or manage period symptoms. But this isn’t the case for all groups. African American women have a complicated relationship with contraception. The shameful history of abuse, mistreatment, and discriminatory policies have been used to control the bodies of women of color and have led many African American women to be distrustful of contraception.
But understanding your choices is vital to making an informed decision about your reproductive health so you can have a safe pregnancy and birth if and when the time comes.
So here is what you really need to know about the history of birth control in the African American community and a rundown of the available birth control options.
Control of Reproductive and Sexual Health of African American Women
Birth control used consistently and correctly prevents unplanned pregnancies and helps with family planning. So why is the relationship with contraception so complex for African American women?
It originates from the inhumane 246-year enslavement of African people in the United States, where women often experienced legalized sexual and reproductive exploitation.
Enslavers and other white men sexually assaulted about 58 percent of all enslaved women between 15 to 30 years old. And because the laws of the time considered enslaved women as property, African American women did not have any legal protection from the assaults.
In addition, enslavers valued and depended upon Black women to bear children to preserve their economic wealth. This suggested that their reproductive profitability mattered more than their bodily autonomy.
Limited Access to Medical Care
Historically, enslaved African American women had limited access to healthcare. And when care was available, these women were often subjected to medical experimentation. François Marie Prevost, a slaveholding surgeon, pioneered cesarean section surgeries on the bodies of Black women. Likewise, James Marion Sims perfected the surgical technique to repair obstetrical fistulas by experimenting on Black women.
These instances of gruesome mistreatment within the origins of American gynecology still influence the present-day health choices of many African American women.
Exploitation During the Civil Right Era
Even with the Emancipation Proclamation in place, which granted freedom to the enslaved, health care, like many other sectors, remained a separate space where Black people were mistreated. Racial disparities in healthcare should have disappeared with the implementation of the Civil Rights Act of 1964, but thousands of poor Black women endured forcible sterilization under various federally funded programs. Driven by the bogus “science” of eugenics, states ordered sterilizing women they deemed”undesirable.” Women were often threatened with termination of their Welfare benefits or denied medical care if they didn’t consent to the procedures.
According to Dorothy Robert, author of the acclaimed novel Killing the Black Body, during this time, sterilization became the most rapidly growing form of birth control, increasing from 200,000 cases in 1970 to 700,000 by 1980.
History of Birth Control in the Black Community
As the availability of birth control options continued to grow, so did the efforts to control Black bodies. Throughout the 1990s, there was increasing concern about women using illicit drugs during pregnancy. Deemed morally deviant and unfit for motherhood, many states introduced aggressive policies and legislative bills encouraging primarily poor, young, addicted Black women to have the Norplant device placed. Hailed as the “first major birth control breakthrough” since the pill, this low-dose birth control contained six flexible capsules, which were inserted under the skin of the upper arm.
Norplant was regarded as the ideal contraceptive since it was long-acting, effective, and once inserted, women were protected against pregnancy for up to five years. More importantly, however, policymakers and legislators embraced this contraceptive as the solution to curb the growing birth rate of “crack babies” (children exposed to crack cocaine in utero). Robert, the author of the novel Killing the Black Body, reports that officials also believed this device would reduce the burden on social programs by limiting the number of poor, young mothers who “deliberately” became pregnant to increase their monthly Welfare check.
However, tens of thousands of women filed lawsuits against Norplant’s manufacturer a few years later, who failed to adequately warn about the side effects of irregular menstrual bleeding, nausea, headaches, and difficult removal.
Available Birth Control Options
African American women have felt the historical trauma and endured unimaginable conditions, procedures, and events that have made it difficult for some to move beyond the negative perceptions of birth control. But with many options available and their proven benefits, it is essential to know all your choices to decide whether birth control is right for you and, if so, which one is the right fit. In addition, understanding the advantages and disadvantages of each option can make you more confident about making an informed decision.
Hormonal Birth Control Methods
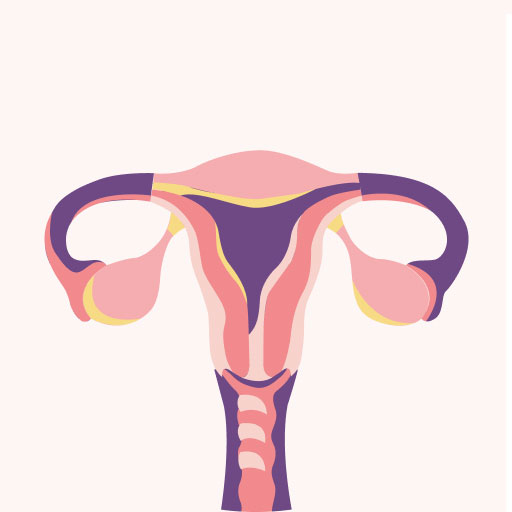
Hormonal birth control prevents your ovaries from releasing eggs and/or thickens your cervical mucus so sperm can’t get through.
Several hormonal methods are available, including:
Hormonal Intrauterine Device (IUD): This T-shaped device is placed inside your uterus by a health provider and releases a small amount of progestin each day to prevent pregnancy. The hormonal IUD can remain in place for 3 to 8 years, depending on your chosen device (Liletta 7 years and Mirena 8 years). Once you decide you’re ready to start your family, you can have it removed, and you should be able to return to your regular cycle.
You may experience spotting and irregular bleeding during the first 3 to 6 months while using a hormonal IUD. For some women, the IUD stops their period altogether. Other side effects you may experience are headaches, nausea, depression, and breast tenderness.
Implant: The birth control implant is a single thin, flexible progestin-based rod inserted under the skin of your upper arm. This rod can stay in place for over three years. You may experience lighter, heavier, extended periods or bleeding between periods.
Depo Provera: “The shot” contains progestin and prevents ovulation. Depo is given as an injection every three months, so you will continue to see your healthcare provider receive your shot. Most women on Depo will have changes to their period, like more bleeding, spotting between periods, or not having a period at all. Other possible side effects include nausea, weight gain, headaches, and sore breasts.
Combined oral contraceptives: Prescribed by your healthcare provider, the “pill” contains estrogen and progestin hormones. You take your pill at the same time each day. Combined hormonal pills come in a 21–day pill pack or as a 23, 24, or 28–day pill pack. There is also a 90-day pill pack of combined hormonal pills called seasonique.
Progestin-only birth control pills: Unlike combined pills, the “mini-pill” only contains the hormone progestin. You take this pill at the same time each day for maximum effectiveness. If you miss taking your medicine by more than 3 hours, use a backup method like a condom for the next 48 hours.
Transdermal Patch: This prescribed adhesive patch is worn on your lower abdomen, buttocks, or upper body. It releases the hormones progestin and estrogen into your body. You wear one patch for a week at a time for a total of 3 weeks. Don’t wear a patch during the fourth week; you will have your period. After week 4, put on a new patch and repeat the cycle. Put your patch on the same day of the week, even if you still are bleeding.
Hormonal Vaginal Contraceptive Ring: The ring is inserted inside your vagina, releasing the hormones progestin and estrogen. You wear the ring for three weeks and take it out for the fourth week to have your period. You will then put in a new ring once your period is over. There is also the annovera, an extended-length ring that lasts up to a year.
After starting combined hormonal contraceptive methods like the “pill,” patch, or ring, you may experience headaches, nausea, sore breasts, spotting, or changes to your period, like it coming early, late, or stopping altogether.
These methods are generally safe but are associated with a small increased risk of blood clots, heart attack, and stroke. This risk is higher if you are over 35 years old and smoke more than 15 cigarettes daily. Having multiple risk factors for cardiovascular disease like high cholesterol, high blood pressure, diabetes, or a history of migraine headaches also increases your risk, especially if not well controlled.
Emergency Contraception: Emergency contraception helps prevent pregnancy after unprotected sex or if your birth control method fails or is not used during sex. It is important to note that emergency contraception isn’t meant to be used as a routine birth control option.
Emergency contraceptive pills (Plan B, Ella) are more effective the sooner you take them but can be used up to five days after unprotected sex. Some emergency contraceptive pills (Plan B) are available over the counter without a prescription. The copper IUD (ParaGard) can also be used as an emergency contraceptive if it’s inserted within five days after unprotected sex.
Non-hormonal Birth Control Options
Non-hormonal birth control doesn’t affect your hormones. It works to prevent pregnancy by decreasing the sperm’s ability to join an egg. Some hormone-free options like condoms, sponges, and diaphragms create physical barriers to prevent pregnancy, while others, like the copper IUD, makes the uterus a hostile place so the fertilized egg can’t implant.
Here is an overview of non-hormonal options:
Copper IUD: The copper IUD (Paragard) is the most effective hormone-free contraception. It is inserted into your uterus, and once in place, this “T” shaped device can remain in place for up to 10 years or until you are ready to take it out. Once removed, your regular cycle should return. During the first few months with your IUD, you may experience side effects like cramps, bleeding, or bleeding between periods. But, these symptoms could go away within a year.
Condoms: Condoms are available with or without spermicide and are worn internally (in the vagina) or externally (over the penis). The external condom is a thin sheath of latex (rubber), polyurethane (plastic), or natural (animal) membrane. The internal condom (a thin plastic pouch) lines the vagina. It is held in place by a closed inner ring near the cervix and an outer ring at the opening of the vagina.
Using a condom consistently and correctly can significantly reduce your risk of sexually transmitted infections (STIs), including HIV. Spermicide use has been associated with increased HIV and STI transmission, especially if used several times a day.
Diaphragm, Cervical Cap, Sponge
Diaphragm: This reusable dome-shaped cup fits inside your vagina and covers your cervix. The diaphragm is made of latex or silicone. A traditional diaphragm comes in different sizes that your healthcare provider must fit. The newer diaphragm (Caya) is one-size-fits-all. All diaphragms must be used with spermicide and left in place for 6 hours after sex but no more than 24 hours total.
The cervical cap: Prescribed and fitted by your healthcare provider, is a small, flexible rubber cap that fits tightly over the cervix to block sperm. Like the diaphragm, the cervical cap should be used with a spermicide and left in place for 6 hours after sex, but no more than 48 hours total.
See your provider to refit your cervical caps after pregnancy, weight loss, weight gain, or a vaginal birth since the fit may change. The cervical cap is less effective in preventing pregnancy for women who have already given birth.
The Sponge: This soft round foam that contains spermicide covers your cervix to block sperm. It can be placed up to 24 hours before sex and left in place for at least 6 hours after sex. You should not wear the sponge for more than 30 hours total. The sponge is less effective in preventing pregnancy in women who have given birth.
Fertility awareness tracking: On average, 12 to 24 percent of women will become pregnant using the fertility awareness method each year. You can prevent pregnancy by knowing and recognizing when you are most fertile each month to avoid having sex during this period. Utilizing a period tracker on a mobile device or manually tracking with a calendar will help if you choose this method.
Things to Consider When Selecting a Birth Control Method
Choosing a birth control method is an important decision. And honestly, the best decision is the one that complements your lifestyle and needs. Generally, birth control poses few serious health risks, but each method has pros and cons. Different factors may influence your decision over your lifetime, like:
- Your age
- Side effects
- Cost and how you will pay for it
- Your reproductive goals (the number of children you want and how soon you want to get pregnant)
- Relationship factors (marital status, number of sexual partners, how often you have sex, and partner preferences)
- Religious beliefs
You should always feel in control of your reproductive health. If you believe your healthcare provider is not respecting your preferences, needs, or concerns, it’s okay to find another provider. By setting clear goals, communicating openly and honestly, and providing your doctor with feedback, you can become your own advocate and have more confidence in your choices.
Birth Control and Your Future
The legacy of slavery, medical experimentation, and suboptimal medical care has contributed to African American women’s long-standing distrust of birth control. Designing policies and a healthcare system that addresses racism, bias and no longer exploits marginalized communities can help repair and restore this fragmented relationship. And as a result, African American women can finally have control over their bodies and reproductive outcomes.