Understanding Heavy Flow: Everything You Need to Know
Let’s talk about something many of us experience but seldom discuss openly—heavy menstrual flow. You know, those times when your period feels more like a relentless tide than a manageable stream. It’s not just “one of those things” to brush off. Together with The Honey Pot Company, Health in Her HUE (HIHH) is here to unpack what a heavy flow really means, why it happens, and how you can manage it with more confidence.

What is Heavy Flow?
Do you often find yourself changing your tampon or pad more frequently than friends or family? Or maybe you’re doubling up with a tampon and pad, and still dealing with leaks. If your period lasts more than a week or if waking up at night to change your protection has become routine, you might be dealing with heavy menstrual flow or menorrhagia. Dr. White, an Obstetrics and Gynecology specialist and Pulse Expert at The Honey Pot Co, breaks it down: “A heavy flow can be defined by the number of days of bleeding and or the amount of blood that occurs during the cycle. A menstrual period that lasts longer than seven days is considered a heavy period.” In addition, experiencing clots, soiling your clothes, or needing to change one tampon or pad more than every 1-2 hours is considered heavy. Also, needing to wear more than one protective item—such as both a tampon and pad at the same time—is considered heavy. Very often, we might not notice that our experiences with our periods are not what is considered “normal.” We invite you to take note and track your experiences over the course of your periods to determine if you may be experiencing a heavy flow.
Common Causes of Heavy Flow
The biggest question many of us might have is, “What causes a heavy flow?” Several health issues can intensify and kick your flow into overdrive. Conditions that affect the structure of your uterus, such as fibroids, uterine polyps, and adenomyosis, are common culprits. Hormonal imbalances like PCOS, hypothyroidism, or hyperthyroidism can also lead to abnormal uterine bleeding. Certain medications, such as the hormone-free IUD (Paragard) or the progesterone birth control implant (Nexplanon), may also contribute to heavier cycles. Dr. White explains, “Fibroids and polyps have extra blood vessels and tissue that can cause heavier cycles, and when there are abnormal levels of certain hormones, this can lead to a heavier flow.” Less commonly, conditions like Von Willebrand’s disease or even precancerous or cancerous cells in the cervix or uterus may be the cause of abnormal bleeding.
Getting the Right Diagnosis
Experiencing a heavy flow can be scary, especially when the cause is not clear. This is why getting more informed about what is causing your heavy flow is important. Getting the right diagnosis can be done in a multitude of ways. Dr White notes, “A pelvic ultrasound is typically the first line of defense to evaluate the uterus and ovaries. This may include an ultrasound probe that goes into the vaginal opening and or on the abdomen. A saline-infused sonohysterogram may also be performed, which is an ultrasound where fluid is injected into the uterus to evaluate the inner lining. In some cases, [an] MRI may be performed for a more detailed evaluation, as well as an endometrial biopsy of the inner uterine layer may be done to rule out cancerous causes.”
To effectively manage heavy flow, it’s important to understand what’s causing it. Here’s what your doctor might suggest during an evaluation:
- Physical Exam: A thorough physical exam, including a speculum exam, to check for any abnormalities in the vagina and cervix.
- Bimanual Exam: This is done to evaluate the uterus and its relation to the other pelvic organs.
- Pap Smear or HPV Test: To ensure there are no abnormal or precancerous cells on the cervix.
- Blood Tests: These check for anemia or blood clotting issues.
- Hormone Levels: To identify any hormonal imbalances that could be contributing to the heavy bleeding.
- Diagnostic Imaging: Your doctor may use pelvic ultrasounds (both transvaginal and abdominal), saline-infused sonohysterograms, or even MRIs to take a closer look at the uterus and ovaries.
- Endometrial Biopsy: This may be scheduled to rule out more serious conditions, such as cancer.
Experiencing heavy flow? Connect with culturally sensitive providers through the HIHH provider directory to find the right care and schedule an appointment.
Managing the Impact
Living with a heavier flow can be inconvenient. It can also lead to significant issues like anemia and severe pain, not to mention the stress it adds to your mental and emotional well-being. According to Dr. White, although stress might slightly alter your menstrual cycle’s timing, it is less likely to affect the flow’s heaviness. Recent research suggests that many women with heavy flow don’t realize it’s abnormal because they lack comparisons. This is why it is important to document your experience, with examples and maybe even photos to share with your healthcare provider. Lacking examples and documentation can delay the diagnosis of conditions like endometriosis, adenomyosis, and hormonal imbalances, which are often underlying causes of heavy flow. Historically, people didn’t talk much about their menstrual cycles, so it was hard to know what was “normal.” With better menstrual products, it became easier to see differences between “light days” and “heavy days.”
Proactive Health Management
Furthermore, it’s important to remember that our experiences as women, especially Black women and women of color, can sometimes mean facing greater challenges in getting the right diagnosis and treatment due to disparities in healthcare access. Therefore, being proactive during medical appointments is key. Dr. White stresses the importance of asking detailed questions and expressing concerns directly.
“Some of the best questions to ask are follow-up questions. Sometimes, you may be told something at a doctor’s appointment and are too nervous to ask for further clarification. Or you may be nervous about a question being too silly. However, there are no wrong questions. The doctor’s appointment is the perfect time to address any of your concerns. Write down your questions and bring them with you. If additional questions come up after the appointment, don’t hesitate to message the doctor. If something is concerning you, use words that express your alarm, like ‘I’m concerned,’ ‘I’m worried,’ or ‘This scares me.’ We are trained specifically to address those fears. If you feel you are not being heard, say so at the time. Ask what signs would make the provider worried so you know what to look out for.”
It’s also important to remember that seeking a second opinion is not only acceptable but often encouraged. If your concerns persist or if you feel uncertain about your diagnosis or treatment plan, getting another perspective can be incredibly valuable. A second opinion can either reaffirm your current course of action or open up alternative treatment options that may not have been considered. Don’t hesitate to ask another provider for a fresh set of eyes, especially if something doesn’t feel right. The goal is always your health and well-being, and any good doctor will understand that getting a second opinion is a proactive step in ensuring you receive the best care possible.
Whether it’s clarifying a diagnosis, exploring additional treatment options, or simply confirming that you’re on the right path, seeking a second opinion is a powerful way to advocate for your health. You deserve to feel confident and comfortable with your care, so never be afraid to explore all your options.
Follow-up and Continuous Care
Following up with regular check-ups is crucial. Dr. White advises, “When coming to your doctor’s appointment, be sure to bring a log of your menstrual cycle, associated symptoms and when they occur, how often you get a cycle, medications you have recently taken, and your sexual health history.”
Also, understand the side effects of common treatments like birth control, which can include nausea, breast tenderness, and mood changes. “Birth control tends to be a commonly used method to help with heavy bleeding. This includes the birth control pill, patch, ring, depo, IUD, or implant such as Nexplanon. Most of these options are not linked with weight gain and are safe to use with other types of medications,” Dr. White points out. It’s important to track your flow over the course of years, even if the flow lightens up after you have found a solution. Understanding your body’s needs and full diagnoses can be helpful during the entire course of your period, from the first period even into menopause.
Practical Tips for Everyday Management
Managing heavy flow may involve adjusting medications, using NSAIDs like ibuprofen to reduce bleeding and alleviate pain, or opting for less processed, iron-rich foods to help manage inflammation. Interesting, right? What you eat matters, too. If you struggle with fibroids, it can be helpful to avoid foods that are highly inflammatory, like red meat. Likewise, low vitamin D has also been linked to worsened fibroids, so adding this supplement to your wellness routine may be beneficial for managing symptoms.
Finding Community and Support
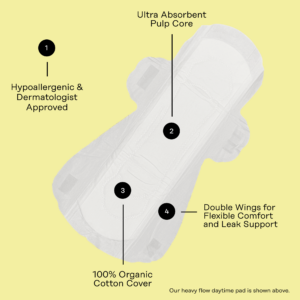
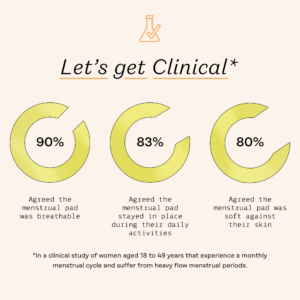
You’re not in this alone. Organizations like The White Dress Project and the Fibroid Foundation can offer support and information. Another great way to receive support is through community and sharing your experiences with friends and family for social support. The Honey Pot Company also provides products, such as its organic and non-herbal-infused pads and tampons, designed specifically for heavy-flow days. These ensure you feel secure and comfortable throughout your cycle.
Explore The Honey Pot Company’s Heavy Flow Collection here for effective solutions.
Conclusion
Understanding and managing heavy menstrual flow centers on confidence, education, and proactive care. Increased dialogue and awareness can significantly improve your quality of life. If you suspect a heavy flow, don’t hesitate to seek professional advice and explore all available treatment options.
For more insights and to connect with healthcare providers who understand, check out the HIHH Provider Directory, join the HIHH Community Forums, explore HIHH Care Squads, or watch on-demand video answers to your burning reproductive health questions through HIHH’s newest feature, Carepoint.
More Content
Mental & Behavioral Health
Part 2: How PMDD Affects the Brain
Psychiatric and medical doctors have some overlapping...
Reproductive & Sexual Health
What to Know About Self-Managed Abortions and Resources to Support
What is self-managed abortion? Self-managed abortion is...